Hepatitis A: Symptoms, Treatments, Medications and Prevention
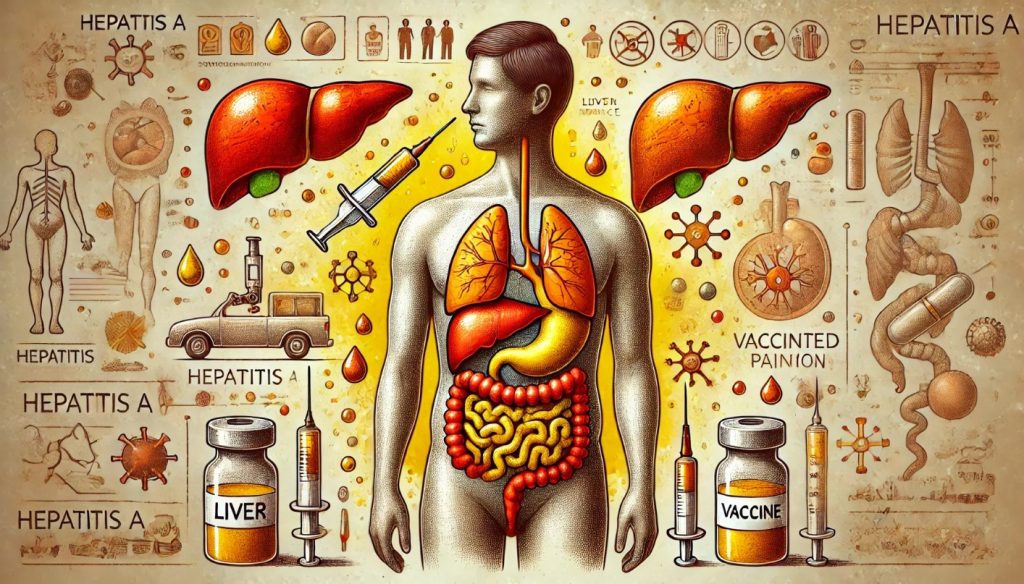
Hepatitis A is a viral liver infection caused by the hepatitis A virus (HAV). It is one of several types of hepatitis viruses that affect the liver, but it is unique because it is often transmitted through contaminated food or water, unlike other types of hepatitis that are spread through blood or other body fluids. Hepatitis A is generally considered a short-term illness, but it can cause severe symptoms in some cases. While it does not typically lead to chronic liver disease like hepatitis B or C, it can still cause considerable health issues, especially in individuals with pre-existing liver conditions.
What is Hepatitis A?
The Hepatitis A Virus
Hepatitis A is caused by the hepatitis A virus (HAV), a single-stranded RNA virus that belongs to the family Picornaviridae. This virus primarily infects the liver and can lead to inflammation and impairment of liver function. Unlike hepatitis B or C, which can result in long-term, chronic infections, hepatitis A is an acute illness, meaning it typically does not last long, and the body eventually clears the virus on its own.
How Hepatitis A Spreads
Hepatitis A is primarily transmitted through the fecal-oral route, meaning the virus is ingested through contact with food, water, or surfaces that have been contaminated with the feces of an infected person. The virus can spread quickly in environments with poor sanitation or inadequate water treatment systems, making it particularly prevalent in areas where hygiene practices may be insufficient.
Common Ways Hepatitis A is Transmitted:
- Contaminated Food and Water: Ingesting food or drinks that have been handled by someone infected with hepatitis A or that have been contaminated by feces containing the virus.
- Person-to-Person Contact: Close personal contact with an infected person, including household contact, sexual contact, or caring for someone with hepatitis A, can result in transmission.
- International Travel: Travelers to countries with high hepatitis A rates are at risk of exposure if they consume contaminated water or food.
- Improper Sanitation: In areas with poor sanitation, hepatitis A can spread through communal living spaces, crowded urban areas, or schools, particularly if clean water is scarce.
Who is at Risk of Hepatitis A?
While anyone can contract hepatitis A if exposed to the virus, certain groups of people are more vulnerable based on their lifestyle, occupation, or living conditions. Understanding who is at higher risk is crucial in implementing effective prevention strategies.
High-Risk Groups for Hepatitis A
1. Travelers to Countries with High Rates of Hepatitis A
People traveling to countries where hepatitis A is endemic or where sanitation standards are lower are at a higher risk of contracting the virus. High-risk areas include parts of Africa, South Asia, Latin America, and the Middle East. Travelers are more likely to be exposed to the virus through contaminated food and water in these regions.
2. Individuals in Close Contact with an Infected Person
Family members, household contacts, or caregivers of people with hepatitis A are at increased risk of infection. Close personal contact with an infected person, including sharing meals, living spaces, or bathroom facilities, facilitates the spread of the virus.
3. Men Who Have Sex with Men (MSM)
Men who have sex with men (MSM) are at increased risk of hepatitis A because the virus can be transmitted through oral-anal contact during sexual activity. Outbreaks of hepatitis A have been reported among MSM populations in several countries.
4. People Who Use Recreational Drugs (Injecting and Non-Injecting)
People who use recreational drugs, whether injecting or non-injecting, are at increased risk of hepatitis A due to the potential for close personal contact with others in environments where sanitation may be inadequate. Sharing drug equipment or living in unhygienic conditions increases the risk of exposure to the virus.
5. Workers in Areas with Poor Sanitation
Occupational risk factors include working in areas with poor sanitation or close contact with potentially contaminated water or waste. This includes food handlers, sewage workers, and healthcare workers who may come into contact with infected individuals or contaminated materials.
6. Individuals with Chronic Liver Disease
Although hepatitis A does not typically lead to chronic liver disease, individuals with pre-existing liver conditions (such as cirrhosis or hepatitis B or C) are at higher risk of severe complications or death if they contract hepatitis A. Their livers are less capable of handling the additional stress caused by an infection.
7. People Living in Overcrowded Conditions
Overcrowded living conditions, such as those found in refugee camps, prisons, or temporary shelters, can facilitate the rapid spread of hepatitis A due to shared facilities and limited access to clean water.
Symptoms of Hepatitis A and How It Is Diagnosed
Hepatitis A symptoms typically appear 2 to 6 weeks after exposure to the virus. Symptoms can range from mild to severe, and some people, especially young children, may not exhibit any symptoms at all. When symptoms do occur, they usually develop suddenly and can last anywhere from several weeks to a few months.
Common Symptoms of Hepatitis A
1. Fatigue
Fatigue is often one of the first symptoms of hepatitis A. Patients may feel tired or weak and have difficulty carrying out their normal daily activities.
2. Nausea and Vomiting
Nausea and vomiting are common, particularly in the early stages of the infection. These symptoms can make it difficult for patients to eat or drink, leading to dehydration.
3. Abdominal Pain and Discomfort
Patients often experience pain or discomfort in the upper right side of the abdomen, where the liver is located. This pain may be dull or sharp, depending on the severity of liver inflammation.
4. Loss of Appetite
Loss of appetite, coupled with nausea and vomiting, can lead to unintentional weight loss during the course of the illness.
5. Jaundice (Yellowing of the Skin and Eyes)
As the liver becomes inflamed, it may fail to process bilirubin (a substance produced during the normal breakdown of red blood cells), leading to a yellowing of the skin and eyes, a condition known as jaundice.
6. Dark Urine
Dark-colored urine is another common symptom caused by the buildup of bilirubin in the blood, which is eventually excreted through the kidneys.
7. Pale Stools
Stools may become pale or clay-colored as bile production is impaired by liver inflammation.
8. Fever
A mild fever often accompanies the initial onset of symptoms, especially in the early stages of the infection.
9. Joint Pain
Some individuals experience joint pain, which can add to the discomfort of the illness.
10. Itchy Skin
Pruritus, or itching of the skin, may occur in some patients as a result of bile salts accumulating in the skin.
How Hepatitis A Is Diagnosed
Diagnosing hepatitis A typically involves a combination of clinical examination and laboratory tests. The healthcare provider will assess the patient’s symptoms and risk factors, such as recent travel or close contact with an infected person. Laboratory tests are used to confirm the presence of hepatitis A and rule out other types of hepatitis or liver diseases.
1. Blood Tests for Hepatitis A
Blood tests are used to detect specific markers of hepatitis A infection, including:
- IgM Anti-HAV (Immunoglobulin M Antibodies): The presence of IgM antibodies indicates a current or recent hepatitis A infection. These antibodies are typically detectable shortly after symptoms begin and persist for several months.
- IgG Anti-HAV (Immunoglobulin G Antibodies): IgG antibodies appear later in the course of the infection and remain in the body for life, providing long-term immunity against hepatitis A. The presence of IgG antibodies without IgM suggests a past infection or vaccination.
2. Liver Function Tests (LFTs)
Liver function tests are commonly used to assess the extent of liver damage and inflammation. Elevated levels of liver enzymes, such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST), indicate liver inflammation, which is characteristic of hepatitis.
3. Bilirubin Levels
Elevated bilirubin levels in the blood are a hallmark of liver dysfunction and are responsible for the jaundice seen in many hepatitis A patients.
4. Physical Examination
A physical examination may reveal signs of jaundice, abdominal tenderness (particularly over the liver), and other symptoms associated with hepatitis A.
Treatments for Hepatitis A
There is no specific treatment for hepatitis A, as it is a self-limiting disease, meaning the body will naturally clear the infection over time. Most people recover completely within a few weeks or months, and the liver heals without lasting damage. However, supportive care and symptom management are crucial during the recovery process.
Supportive Care for Hepatitis A
1. Rest
Fatigue is a common symptom of hepatitis A, and getting plenty of rest is essential for recovery. Patients should avoid strenuous activities and allow their bodies the time they need to heal.
2. Hydration
Nausea and vomiting can lead to dehydration, so it’s important to stay hydrated by drinking plenty of fluids. Oral rehydration solutions or electrolyte-rich drinks can help prevent dehydration.
3. Diet Modifications
Eating small, frequent meals can help manage nausea and maintain energy levels. It may be helpful to avoid fatty or greasy foods that can worsen nausea and indigestion.
4. Avoid Alcohol
Since the liver is already inflamed and working hard to fight the virus, consuming alcohol can further damage the liver and slow down recovery. It’s recommended that patients abstain from alcohol until their liver function returns to normal.
5. Over-the-Counter Medications
Acetaminophen (Tylenol) should be used cautiously or avoided altogether, as it can be toxic to the liver. Patients should consult their healthcare provider before using any medications, including over-the-counter drugs, during their illness.
Hospitalization for Severe Cases
In rare cases, hepatitis A can cause severe liver damage (acute liver failure), especially in individuals with pre-existing liver conditions. These patients may require hospitalization for close monitoring and supportive care, such as intravenous fluids or even a liver transplant in the most severe cases.
Most Common Medications for Hepatitis A
Because hepatitis A is typically self-limiting, specific antiviral medications are not necessary. However, symptom management may involve the use of medications to alleviate discomfort or prevent complications.
1. Antiemetics for Nausea and Vomiting
Patients with severe nausea and vomiting may be prescribed antiemetic medications, such as ondansetron (Zofran), to help control these symptoms and prevent dehydration.
2. Pain Relievers for Discomfort
For patients experiencing pain or fever, pain relievers such as ibuprofen (Advil) or acetaminophen (Tylenol) may be recommended. However, acetaminophen should be used with caution due to its potential liver toxicity, especially in patients with liver disease.
3. Intravenous Fluids
In cases where dehydration becomes a concern, intravenous (IV) fluids may be administered in a healthcare setting to help rehydrate the patient.
4. Vitamin and Nutrient Supplements
Patients experiencing prolonged nausea, vomiting, or loss of appetite may be prescribed vitamin and nutrient supplements to maintain adequate nutrition during recovery.
Where is Hepatitis A Most Prevalent?
Hepatitis A is a global disease, but its prevalence varies significantly depending on geographic region, sanitation standards, and access to clean water. It is more common in countries with limited sanitation and hygiene infrastructure, but cases can occur anywhere.
Regions with High Hepatitis A Prevalence
1. Developing Countries
Hepatitis A is most prevalent in developing countries where access to clean water and sanitation is limited. In these regions, children are often exposed to the virus at a young age, typically before the age of 10. While most young children experience mild symptoms, the virus spreads quickly in environments with poor sanitation.
2. Africa
Many parts of Africa, particularly Sub-Saharan Africa, have high rates of hepatitis A infection due to inadequate sanitation, limited access to clean water, and crowded living conditions.
3. South Asia and Southeast Asia
Countries such as India, Bangladesh, Pakistan, and Nepal experience high rates of hepatitis A due to poor sanitation practices and water contamination. Southeast Asian countries such as Vietnam, Thailand, and Indonesia also report high numbers of hepatitis A cases.
4. Latin America
In Central and South America, hepatitis A is common, particularly in rural areas where sanitation and water purification systems may be inadequate.
5. Middle East
Several countries in the Middle East have a moderate to high prevalence of hepatitis A, particularly in areas where refugee populations or internally displaced persons live in crowded conditions with poor sanitation.
Regions with Low Hepatitis A Prevalence
In developed countries, including most parts of North America, Europe, Australia, and Japan, the prevalence of hepatitis A is relatively low due to better sanitation practices, widespread vaccination, and improved hygiene standards. However, travelers from these regions who visit high-risk areas are more vulnerable to contracting the virus if they are not vaccinated.
Prevention of Hepatitis A
Preventing hepatitis A involves a combination of vaccination, good hygiene practices, and ensuring access to clean water. Travelers, in particular, should take precautions when visiting high-risk areas.
1. Hepatitis A Vaccination
The hepatitis A vaccine is the most effective way to prevent infection. The vaccine is typically administered in two doses, six months apart, and provides long-lasting immunity.
Who Should Get Vaccinated?
- Travelers to High-Risk Areas: Anyone traveling to countries where hepatitis A is prevalent should receive the vaccine.
- Men Who Have Sex with Men (MSM): MSM are at increased risk of hepatitis A and should be vaccinated.
- People with Chronic Liver Disease: Those with pre-existing liver conditions should be vaccinated to prevent complications from hepatitis A.
- Healthcare Workers: Healthcare providers who may be exposed to the virus should receive the vaccine.
- Children: In many countries, routine childhood vaccination for hepatitis A is recommended.
2. Good Hygiene Practices
Hand Washing
Frequent and thorough handwashing with soap and water, especially after using the bathroom, changing diapers, and before preparing or eating food, is essential to preventing the spread of hepatitis A.
Avoid Contaminated Food and Water
In areas where hepatitis A is common, travelers should avoid drinking untreated water, consuming raw or undercooked food, and eating food from street vendors. Drinking bottled water and eating food that has been thoroughly cooked and served hot can reduce the risk of infection.
Safe Food Handling
People who handle food, whether at home or in restaurants, should follow proper food safety guidelines to avoid contamination with the hepatitis A virus.
3. Public Health Measures
Improved Sanitation and Access to Clean Water
Governments and public health organizations play a critical role in reducing the prevalence of hepatitis A by ensuring access to clean water, improving sanitation infrastructure, and promoting public health campaigns focused on hygiene practices.