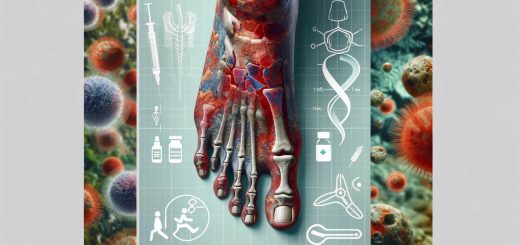
Scalded Skin Syndrome: Symptoms, Treatments, Medications and Prevention
Staphylococcal Scalded Skin Syndrome (SSSS), commonly referred to as Scalded Skin Syndrome, is a rare but serious skin condition caused by toxins produced by the bacteria Staphylococcus aureus. This condition primarily affects infants and young children, although it can occasionally occur in adults, especially those with weakened immune systems. Scalded Skin Syndrome is characterized by widespread red, blistered skin that resembles a burn, and without prompt treatment, it can lead to serious complications.
What is Scalded Skin Syndrome?
Scalded Skin Syndrome is a dermatological condition caused by the release of toxins from a strain of Staphylococcus aureus bacteria, specifically those producing exfoliative toxins. These toxins break down the proteins responsible for holding the outer layer of the skin (epidermis) together, leading to widespread blistering and shedding of the skin. The condition often mimics a severe burn, hence its name.
The skin damage in SSSS occurs due to the exfoliative toxins (exfoliatin A and B), which target the desmoglein-1 protein. Desmoglein-1 is an important component of the skin’s cellular junctions that hold cells together. The disruption of these junctions causes the skin to slough off, leading to large areas of red, raw, and tender skin, similar to a scald burn.
SSSS is primarily an acute condition and requires immediate medical intervention. It is important to note that although the skin is damaged, the deeper layers of the skin, such as the dermis, remain intact, which distinguishes SSSS from conditions like toxic epidermal necrolysis (TEN), where deeper skin layers are affected.
Who is at Risk of Scalded Skin Syndrome?
While Scalded Skin Syndrome can affect people of all ages, certain groups are more vulnerable due to factors such as their immune system, age, and overall health. Understanding the populations at risk can help in early diagnosis and prompt treatment.
Populations at Higher Risk
1. Infants and Newborns
SSSS most commonly affects infants and newborns, particularly those under the age of 6 years, with the highest incidence in children younger than 2 years old. Infants are at higher risk because their immune systems are not fully developed, and they may not yet have strong defenses against bacterial infections like Staphylococcus aureus. Additionally, their skin is thinner and more delicate, making it more susceptible to the exfoliative toxins.
2. Young Children
Children up to the age of 5 are also at increased risk of developing Scalded Skin Syndrome due to their underdeveloped immune systems and increased susceptibility to bacterial infections. In daycare centers or schools, children are more likely to come into contact with others who may carry the bacteria, leading to higher transmission rates.
3. Adults with Weakened Immune Systems
Although rare in adults, Scalded Skin Syndrome can occur in individuals with compromised immune systems. This includes:
- People with chronic illnesses such as kidney disease or diabetes.
- Cancer patients undergoing chemotherapy or radiation therapy, which weakens the immune system.
- HIV/AIDS patients, who have a significantly diminished immune response.
- Organ transplant recipients who are on immunosuppressive medications.
- Patients undergoing long-term steroid treatment, which can suppress the body’s immune defenses.
4. Patients with Skin Infections
SSSS can develop in individuals who have existing skin infections caused by Staphylococcus aureus. In such cases, the bacteria may enter the bloodstream, releasing toxins that spread and damage the skin.
5. Individuals with Poor Hygiene or Overcrowded Living Conditions
Overcrowded living environments and poor hygiene conditions increase the risk of bacterial transmission, including the spread of Staphylococcus aureus. This is particularly concerning in institutional settings such as nursing homes, hospitals, and daycares, where close contact among individuals can facilitate the spread of the bacteria responsible for SSSS.
Behavioral and Environmental Risk Factors
Certain behaviors or environmental factors can increase the risk of contracting Staphylococcus aureus and developing SSSS. These include:
- Direct contact with infected individuals or carriers of Staphylococcus aureus.
- Sharing personal items such as towels, clothing, or bedding that may harbor the bacteria.
- Living in unsanitary conditions or environments with limited access to clean water and hygiene facilities.
Symptoms of Scalded Skin Syndrome
The symptoms of Scalded Skin Syndrome typically begin with a localized bacterial infection, such as impetigo or cellulitis, but rapidly progress as the toxins spread through the bloodstream, affecting large areas of the skin. The progression of SSSS can be alarming, and recognizing the early signs is crucial for timely treatment.
Early Symptoms
In the early stages of SSSS, symptoms may be subtle and resemble those of other bacterial skin infections. Common early signs include:
- Fever: A sudden onset of fever, often with body temperatures exceeding 38°C (100.4°F).
- Redness and Swelling (Erythema): The affected areas of skin may appear red, swollen, and tender.
- Skin Tenderness and Irritation: The skin may feel sore or painful to the touch, even before visible blistering occurs.
- Localized Infection: In some cases, there may be an initial localized infection, such as impetigo, in which small blisters or pustules form in areas such as the face, neck, or groin.
Advanced Symptoms
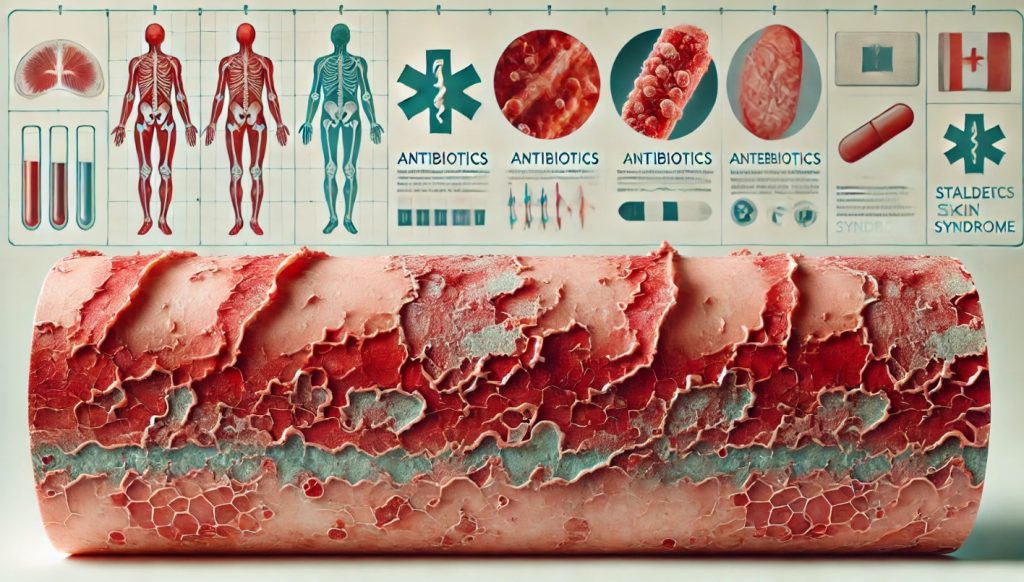
As the condition progresses, the toxins cause widespread skin damage, leading to the following hallmark symptoms of Scalded Skin Syndrome:
1. Widespread Redness (Erythema)
The redness of the skin becomes more widespread, often affecting large areas of the body, including the face, trunk, and extremities. The skin may appear bright red and inflamed, similar to a burn.
2. Blistering
Large, fluid-filled blisters develop over the affected areas. These blisters are fragile and easily rupture, leaving behind raw, moist skin. The blisters are typically thin-walled and may peel away, exposing tender, raw skin beneath.
3. Skin Shedding (Exfoliation)
The affected skin may begin to slough off or peel in sheets, a condition known as exfoliation. This can lead to significant discomfort and increases the risk of secondary infections as the protective outer layer of skin is compromised.
4. Nikolsky’s Sign
One of the diagnostic signs of SSSS is Nikolsky’s sign, in which gentle pressure or rubbing of the skin causes it to peel or slough off. This is a critical indicator of severe skin damage caused by the toxins.
5. Mucosal Involvement (Rare)
In some cases, the mucous membranes (e.g., the mouth, eyes, or genitals) may be affected, leading to dryness, irritation, and redness. However, unlike toxic epidermal necrolysis (TEN), mucosal involvement in SSSS is generally minimal.
Systemic Symptoms
In addition to skin-related symptoms, individuals with SSSS may experience systemic effects due to the spread of toxins. These include:
- Fever and Chills: A high fever is common, accompanied by shaking chills.
- Malaise and Fatigue: Individuals may feel extremely tired or weak due to the body’s response to the infection.
- Dehydration: The loss of skin integrity and fluid from blistering can lead to dehydration, especially in infants and young children.
How is Scalded Skin Syndrome Diagnosed?
Diagnosing Scalded Skin Syndrome involves a combination of clinical examination, laboratory tests, and, in some cases, skin biopsies. Early diagnosis is critical to prevent complications and begin appropriate treatment.
Diagnostic Methods for Scalded Skin Syndrome
1. Physical Examination
A healthcare provider will begin by performing a thorough physical examination, looking for characteristic signs of SSSS, including:
- Widespread redness and blistering of the skin.
- Nikolsky’s sign, where the skin peels away with gentle pressure.
- Presence of localized skin infections, such as impetigo or cellulitis, that may have preceded the onset of SSSS.
The provider will also ask about the patient’s symptoms, including the onset of fever, skin tenderness, and any recent infections.
2. Skin Biopsy
In some cases, a skin biopsy may be performed to confirm the diagnosis of Scalded Skin Syndrome. A small sample of the affected skin is taken and examined under a microscope. The biopsy can help distinguish SSSS from other blistering skin conditions, such as toxic epidermal necrolysis (TEN) or bullous impetigo. In SSSS, the biopsy typically reveals separation of the upper layers of the epidermis (superficial cleavage), while the dermis remains intact.
3. Bacterial Cultures
To identify the presence of Staphylococcus aureus, bacterial cultures may be taken from the original infection site, such as a skin lesion, nasal passages, or blood. Culturing the bacteria can help confirm the presence of a toxin-producing strain of Staphylococcus aureus.
4. Blood Tests
Blood tests may be ordered to assess the patient’s overall health and detect signs of infection or inflammation. Common blood tests include:
- Complete Blood Count (CBC): A CBC can reveal elevated white blood cell counts, which indicate the body’s response to infection.
- C-Reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR): These markers of inflammation are often elevated in bacterial infections like SSSS.
- Blood Cultures: Blood cultures may be taken to detect if the infection has spread systemically (bacteremia). This is particularly important in cases involving immunocompromised individuals or those showing signs of sepsis.
5. Imaging Studies
In severe cases or when complications are suspected, imaging studies like X-rays, ultrasound, or CT scans may be used to assess the involvement of internal organs or to rule out other infections that might complicate the treatment of SSSS.
Differential Diagnosis
SSSS can resemble other skin conditions, so it is important to distinguish it from:
- Toxic Epidermal Necrolysis (TEN): A more severe skin condition where deeper layers of skin are affected, often caused by drug reactions.
- Bullous Impetigo: A localized form of staphylococcal infection where the blisters remain confined to certain areas.
- Contact Dermatitis: An allergic reaction that can cause blistering but does not involve systemic bacterial infection.
Treatments for Scalded Skin Syndrome
Prompt treatment of Scalded Skin Syndrome is critical to prevent complications and to reduce the risk of secondary infections. The primary goals of treatment are to eliminate the underlying bacterial infection, manage skin damage, and provide supportive care to address dehydration and pain.
Antibacterial Therapy
1. Intravenous (IV) Antibiotics
The cornerstone of SSSS treatment is the administration of intravenous antibiotics, which are needed to kill the Staphylococcus aureus bacteria producing the toxins. Antibiotics are usually started immediately, even before the specific bacterial strain is confirmed. Common antibiotics include:
- Nafcillin or Oxacillin: These are beta-lactam antibiotics commonly used to treat infections caused by methicillin-sensitive Staphylococcus aureus (MSSA).
- Vancomycin or Clindamycin: These are used if methicillin-resistant Staphylococcus aureus (MRSA) is suspected or confirmed. Vancomycin is effective against most strains of MRSA, while clindamycin helps reduce toxin production.
The duration of antibiotic treatment usually lasts for 7 to 10 days, depending on the severity of the infection and the patient’s response to therapy.
Supportive Care
In addition to antibiotics, supportive care plays a crucial role in the management of Scalded Skin Syndrome, particularly in infants and immunocompromised patients.
1. Fluid Replacement
Dehydration is a common concern in patients with SSSS due to the significant loss of fluids from the damaged skin. Intravenous fluids are often administered to maintain hydration, electrolyte balance, and blood pressure.
2. Pain Management
Pain management is essential due to the extensive skin damage and sensitivity associated with SSSS. Mild to moderate pain may be managed with oral analgesics such as acetaminophen or ibuprofen. In more severe cases, stronger pain relief may be required, including opioids.
3. Wound Care
The peeling and sloughing of the skin require careful wound care to prevent secondary infections. Wound management may involve:
- Non-Adherent Dressings: To cover the raw, exposed skin without causing further irritation.
- Topical Antibiotics: Mupirocin or silver sulfadiazine may be applied to the affected areas to prevent bacterial colonization.
- Moisturizing Ointments: These help soothe the skin and promote healing by maintaining moisture.
Patients may need specialized care in burn units or intensive care units, especially if the skin damage is extensive or complications arise.
4. Temperature Regulation
Because SSSS causes extensive skin loss, patients may have difficulty regulating their body temperature. Keeping the environment warm and providing thermal blankets can help stabilize body temperature.
Special Considerations for Infants and Children
In infants and young children, treatment may require additional supportive care measures such as frequent monitoring, nutritional support, and infection control measures. Pediatric patients with SSSS are often treated in specialized pediatric care units or burn units where they can receive the appropriate level of care.
Common Medications for Scalded Skin Syndrome
Several medications are commonly used to treat Scalded Skin Syndrome, including antibiotics, pain relievers, and supportive care medications. The choice of medications depends on the severity of the condition and the patient’s age, immune status, and overall health.
- Nafcillin or Oxacillin
- Beta-lactam antibiotics that are first-line treatments for methicillin-sensitive Staphylococcus aureus (MSSA).
- Administered intravenously to rapidly eliminate the bacterial infection.
- Vancomycin
- An antibiotic used to treat methicillin-resistant Staphylococcus aureus (MRSA) infections.
- Particularly important in cases where MRSA is suspected or confirmed.
- Clindamycin
- Often used in conjunction with other antibiotics to reduce the production of staphylococcal toxins.
- Administered either intravenously or orally, depending on the severity of the infection.
- Pain Relievers (Analgesics)
- Acetaminophen or Ibuprofen: Commonly used to manage mild to moderate pain and fever.
- Opioids: May be prescribed for severe pain, especially in cases of extensive skin damage.
- Topical Antibiotics
- Mupirocin or Silver Sulfadiazine: Applied directly to the affected areas to prevent secondary infections and promote healing of the skin.
- Intravenous Fluids
- Essential for preventing dehydration and maintaining electrolyte balance, especially in pediatric patients.
Where is Scalded Skin Syndrome Most Prevalent?
Scalded Skin Syndrome is a relatively rare condition, but it can occur worldwide. Certain populations and regions may see higher incidences of SSSS due to factors such as the prevalence of Staphylococcus aureus infections, access to healthcare, and living conditions.
Global Prevalence
1. Developed Countries
In developed countries, SSSS is most commonly seen in hospitals, neonatal units, and pediatric care centers. Although it is relatively rare, SSSS can occur in outbreaks in healthcare settings due to the transmission of Staphylococcus aureus. Strict hygiene practices and early detection help prevent large-scale outbreaks.
2. Developing Countries
In developing regions where access to clean water, sanitation, and healthcare is limited, infections like impetigo, which can lead to SSSS, may be more common. Overcrowding, poor hygiene, and limited access to antibiotics increase the risk of staphylococcal infections and, consequently, the development of SSSS.
3. Neonatal and Pediatric Units
Neonates and infants in hospital settings, particularly in neonatal intensive care units (NICUs), are more vulnerable to contracting Staphylococcus aureus, which can lead to outbreaks of SSSS. In these cases, close monitoring and strict infection control measures are crucial to prevent the spread.
4. Immunocompromised Populations
Populations with compromised immune systems, including individuals with HIV/AIDS, cancer patients, and transplant recipients, are at a higher risk of contracting SSSS. In these populations, the incidence of SSSS is typically higher in regions with poor access to healthcare services.
Prevention of Scalded Skin Syndrome
Preventing Scalded Skin Syndrome largely involves controlling the spread of Staphylococcus aureus infections and reducing the risk of transmission in high-risk populations. Proper hygiene, infection control, and early treatment of bacterial skin infections are key strategies in preventing SSSS.
Preventive Measures
1. Good Hygiene Practices
Maintaining good hygiene is essential to preventing the spread of Staphylococcus aureus, particularly in healthcare settings, schools, and daycares. Simple measures like frequent handwashing, using alcohol-based sanitizers, and keeping skin wounds clean and covered can help reduce the risk of bacterial transmission.
2. Early Treatment of Skin Infections
Treating skin infections such as impetigo or cellulitis early can prevent the progression to SSSS. Patients with known Staphylococcus aureus infections should seek prompt medical care and follow prescribed antibiotic treatments to avoid complications.
3. Infection Control in Healthcare Settings
Hospitals, neonatal units, and long-term care facilities should implement strict infection control measures, including:
- Isolation of Infected Patients: Patients with confirmed or suspected staphylococcal infections should be isolated to prevent the spread of bacteria to other patients.
- Sterilization of Medical Equipment and Surfaces: Healthcare workers should ensure that all equipment, bedding, and surfaces are properly sterilized to reduce the risk of bacterial transmission.
- Regular Hand Hygiene: Healthcare workers should practice proper hand hygiene before and after caring for patients, especially those with skin infections.
4. Reducing Close Contact in Outbreaks
During outbreaks of staphylococcal infections, it is essential to limit close contact between infected and uninfected individuals. Children with active skin infections should be kept home from school or daycare until they have received treatment.
5. Immunization and General Health
While there is no vaccine specifically for Staphylococcus aureus, maintaining overall health through good nutrition, immunizations, and regular medical check-ups can help bolster the immune system’s ability to fight off bacterial infections.