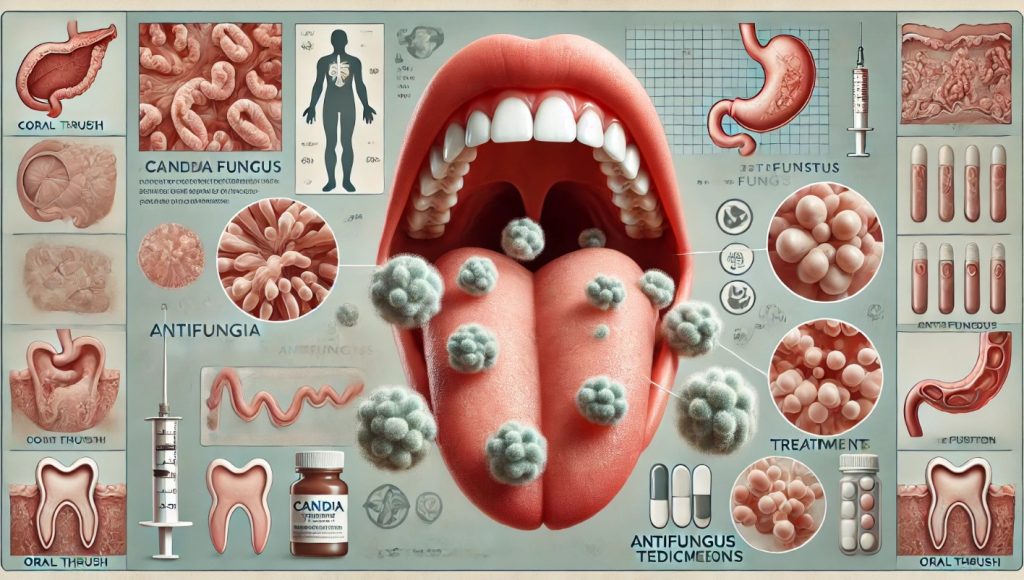
Thrush: Symptoms, Treatments, Medications and Prevention
Thrush, also known as candidiasis, is a fungal infection caused by the overgrowth of Candida species, most commonly Candida albicans. This yeast naturally resides in small amounts on the skin, in the mouth, throat, gut, and genital areas without causing harm. However, when the balance of microorganisms in the body is disrupted, Candida can multiply and cause an infection. Thrush can affect various parts of the body, with the most common forms being oral thrush (in the mouth) and vaginal thrush (in the genital area).
Thrush is typically mild and easily treatable, but it can become severe in certain populations, such as those with weakened immune systems.
Who Is at Risk of Thrush?
Thrush can affect anyone, but certain individuals and groups are at a higher risk due to various factors. These include age, health status, medications, and lifestyle habits that can disrupt the natural balance of microorganisms in the body, leading to the overgrowth of Candida.
Infants and Elderly
Infants and elderly individuals are particularly susceptible to thrush, especially oral thrush, because their immune systems are either underdeveloped (in infants) or weakened (in the elderly). Infants are often exposed to Candida during childbirth or breastfeeding, while older adults may experience weakened immune defenses due to age or chronic conditions.
- Infants: Oral thrush is common in babies under 6 months, especially if they are breastfed. Candida can transfer between the mother’s nipples and the baby’s mouth during breastfeeding.
- Elderly: As the immune system weakens with age, older adults, especially those wearing dentures, are more likely to develop oral thrush.
People with Weakened Immune Systems
Individuals with weakened or compromised immune systems are at a higher risk of developing thrush. This includes:
- HIV/AIDS patients: People living with HIV/AIDS are more susceptible to fungal infections, including thrush, because their immune systems are unable to keep the Candida yeast in check.
- Cancer patients: Those undergoing chemotherapy or radiation therapy are at increased risk of developing thrush due to weakened immunity.
- Organ transplant recipients: People who have had organ transplants and are on immunosuppressive medications to prevent organ rejection are more vulnerable to infections like thrush.
People Taking Certain Medications
Certain medications can disrupt the natural balance of microorganisms in the body and increase the risk of Candida overgrowth, leading to thrush. These medications include:
- Antibiotics: Broad-spectrum antibiotics kill both harmful and beneficial bacteria, which can allow Candida to multiply unchecked.
- Corticosteroids: Oral and inhaled corticosteroids, often used for conditions like asthma or autoimmune diseases, can increase the risk of oral thrush by weakening the body’s defense mechanisms.
- Chemotherapy drugs: These drugs can compromise the immune system, making it harder for the body to control Candida growth.
Diabetics
People with uncontrolled diabetes are at higher risk of developing thrush. High blood sugar levels can provide an ideal environment for Candida growth, and a weakened immune response in diabetics makes it more difficult to fight off infections.
Individuals with Poor Oral Hygiene or Dry Mouth
Oral thrush is more likely to develop in people with poor oral hygiene or conditions that cause dry mouth (xerostomia). Dry mouth reduces saliva production, which helps control the growth of fungi in the mouth.
- Dentures: People who wear dentures, particularly if they are not properly fitted or cleaned regularly, are more susceptible to oral thrush.
- Smoking: Smoking can also increase the risk of oral thrush due to its effects on oral health and immunity.
Pregnant Women
Pregnant women are more prone to developing vaginal thrush due to hormonal changes that affect the balance of bacteria and yeast in the body. The increased estrogen levels during pregnancy promote the growth of Candida in the vaginal area.
Symptoms of Thrush
The symptoms of thrush vary depending on the area of the body affected by the infection. The most common types are oral thrush and vaginal thrush, though Candida can infect other parts of the body, such as the skin and throat. In severe cases, the infection can become systemic, especially in immunocompromised individuals.
Oral Thrush
Oral thrush affects the mucous membranes in the mouth and throat, and its symptoms can range from mild discomfort to more severe complications.
Common Symptoms
- White patches: Creamy white or yellowish patches on the tongue, inner cheeks, gums, tonsils, or roof of the mouth are the hallmark of oral thrush. These patches may bleed slightly if scraped or rubbed.
- Redness and soreness: The affected areas in the mouth may become red, inflamed, and painful, making it difficult to eat or swallow.
- Loss of taste: Some individuals may experience a reduction in their ability to taste food.
- Cracked corners of the mouth: Cracks or sores, known as angular cheilitis, may develop at the corners of the mouth.
- Difficulty swallowing: In more severe cases, oral thrush can extend down the throat (esophageal candidiasis), causing pain and difficulty swallowing.
Vaginal Thrush
Vaginal thrush (also known as vulvovaginal candidiasis) affects the vaginal area and can cause a range of uncomfortable symptoms.
Common Symptoms
- Itching and irritation: Intense itching and irritation in and around the vagina are common signs of vaginal thrush.
- Thick, white discharge: Vaginal thrush often causes a thick, white, cottage cheese-like discharge. Unlike bacterial infections, the discharge typically does not have a strong odor.
- Redness and swelling: The vaginal area may become red, swollen, and tender to the touch.
- Burning sensation: A burning sensation, particularly during urination or intercourse, is often reported.
Skin and Nail Infections
Candida can also infect the skin, particularly in moist, warm areas of the body, such as skin folds, the armpits, groin, and under the breasts. Symptoms of cutaneous candidiasis include:
- Red, itchy rash: The skin becomes red, irritated, and itchy, with possible pustules or small blisters.
- Cracked or sore skin: Infected areas may become cracked, sore, or weepy.
- Fungal nail infections: Candida can also infect the nails, causing them to become thickened, discolored, and brittle.
Systemic Candidiasis
In rare cases, Candida can enter the bloodstream and spread to other organs, leading to a severe and potentially life-threatening condition known as systemic candidiasis or invasive candidiasis. This occurs primarily in people with weakened immune systems, such as those with HIV/AIDS, cancer, or undergoing organ transplants. Symptoms include:
- Fever and chills: Persistent fever and chills that do not improve with antibiotics may indicate a systemic Candida infection.
- Organ dysfunction: Depending on the organs affected, systemic candidiasis can cause symptoms of organ failure, such as difficulty breathing, chest pain, or altered mental state.
Diagnosis of Thrush
Thrush is typically diagnosed through a combination of physical examination and laboratory tests. Early diagnosis and treatment are important to prevent the infection from spreading or becoming chronic.
Physical Examination
A healthcare provider will begin by examining the affected area for visible signs of thrush, such as white patches in the mouth or vaginal discharge. The appearance of these symptoms often provides enough information for a clinical diagnosis.
Microscopic Examination
To confirm the diagnosis, a sample of the affected tissue may be taken and examined under a microscope. For oral thrush, this might involve scraping some of the white patches from the mouth, while for vaginal thrush, a swab of the vaginal discharge may be collected.
- KOH (potassium hydroxide) test: This test involves applying a potassium hydroxide solution to the sample, which dissolves the surrounding tissue and leaves fungal cells intact for easy viewing under a microscope.
- Gram stain: A Gram stain may also be used to help visualize Candida yeast cells.
Fungal Culture
In some cases, particularly if the infection is severe or recurrent, a healthcare provider may order a fungal culture to identify the specific species of Candida causing the infection. This involves placing the sample in a medium that encourages fungal growth. A culture can help determine the best course of treatment, particularly if there is resistance to common antifungal medications.
Blood Tests
In cases of systemic candidiasis, blood tests are often necessary to detect the presence of Candida in the bloodstream. Blood cultures may be taken to identify the specific fungal species, and additional tests, such as a complete blood count (CBC) or other immune function tests, may be ordered to assess the severity of the infection and the overall health of the patient.
Endoscopy
If esophageal thrush (thrush that extends down the throat) is suspected, a doctor may perform an endoscopy to examine the esophagus, stomach, and part of the small intestine. This involves using a flexible tube with a light and camera (endoscope) to look for signs of Candida infection.
Treatments for Thrush
The treatment of thrush depends on the location of the infection, its severity, and the patient’s overall health. Most cases of thrush can be treated with antifungal medications, but the approach may vary based on the type of thrush and the patient’s risk factors.
Antifungal Medications
Antifungal medications are the mainstay of treatment for all forms of thrush. These medications work by inhibiting the growth of Candida and eliminating the infection. Antifungals can be applied topically or taken orally, depending on the severity and location of the infection.
- Topical treatments: For mild cases of oral or vaginal thrush, topical antifungal medications, such as creams, ointments, or lozenges, are often sufficient.
- Oral antifungals: More severe or widespread infections may require oral antifungal medications, which are taken in pill or liquid form to treat the infection from the inside out.
Oral Thrush Treatment
Oral thrush is typically treated with topical antifungals applied directly to the affected area. Common treatments include:
- Nystatin oral suspension: Nystatin is often prescribed as a liquid that is swished around the mouth and then swallowed. It is typically used 4 times a day for 7 to 14 days.
- Clotrimazole lozenges: These antifungal lozenges dissolve in the mouth, slowly releasing the medication. They are used several times a day for 1 to 2 weeks.
- Fluconazole (oral): For more severe or resistant cases, fluconazole, an oral antifungal medication, may be prescribed. A typical course lasts for 7 to 14 days.
Vaginal Thrush Treatment
Vaginal thrush is treated with antifungal medications that can be applied topically or taken orally. Common treatments include:
- Miconazole: Miconazole is available as a cream or suppository that is inserted into the vagina for 1 to 7 days, depending on the severity of the infection.
- Clotrimazole: This antifungal is available in cream or suppository form and is used in a similar way to miconazole.
- Fluconazole (oral): For more severe or recurrent vaginal thrush, oral fluconazole may be prescribed as a single dose or in a longer regimen over several days.
Systemic Candidiasis Treatment
Systemic candidiasis is a serious condition that requires immediate medical attention and aggressive treatment. Treatment typically involves:
- Intravenous antifungal medications: In cases of systemic candidiasis, antifungal medications such as amphotericin B or echinocandins (e.g., caspofungin, micafungin) are administered intravenously in a hospital setting.
- Long-term antifungal therapy: For people with weakened immune systems, such as those with HIV/AIDS or undergoing chemotherapy, long-term antifungal therapy may be necessary to prevent recurrent infections.
Treating Recurrent Thrush
Some individuals, particularly those with underlying health conditions such as diabetes or compromised immune systems, may experience recurrent thrush. In such cases, long-term antifungal treatment or regular preventive measures may be necessary.
- Fluconazole: Oral fluconazole may be prescribed in a weekly or monthly regimen to prevent recurrence.
- Probiotics: Some healthcare providers may recommend probiotics to help restore the natural balance of bacteria and yeast in the body, although more research is needed to confirm their effectiveness in preventing thrush.
Common Medications for Thrush
Several antifungal medications are used to treat thrush, depending on the severity of the infection and the location. These medications work by targeting the Candida yeast and inhibiting its growth.
Nystatin
- Dosage: Nystatin is commonly prescribed for oral thrush as a liquid suspension. The typical dosage is 4 mL of suspension 4 times daily, swished in the mouth and swallowed.
- Effectiveness: Nystatin is effective for treating mild to moderate cases of oral thrush.
- Side effects: Nystatin is generally well-tolerated but may cause mild gastrointestinal discomfort or irritation in the mouth.
Fluconazole
- Dosage: Fluconazole is available as an oral tablet or liquid. For oral thrush, the usual dose is 100-200 mg once daily for 7 to 14 days. For vaginal thrush, a single 150 mg oral dose is often prescribed.
- Effectiveness: Fluconazole is highly effective for treating both oral and vaginal thrush, as well as systemic candidiasis.
- Side effects: Common side effects include nausea, headache, and abdominal pain. In rare cases, fluconazole can cause liver toxicity, so it may require monitoring in high-risk patients.
Clotrimazole
- Dosage: Clotrimazole is available as lozenges (troches) for oral thrush and as vaginal suppositories or creams for vaginal thrush. The typical dosage for lozenges is 1 troche (10 mg) dissolved in the mouth 5 times daily for 1 to 2 weeks.
- Effectiveness: Clotrimazole is effective for mild to moderate cases of thrush, especially in topical form.
- Side effects: Common side effects include irritation or burning at the application site.
Miconazole
- Dosage: Miconazole is available as a vaginal cream, suppository, or oral gel. For vaginal thrush, it is applied once daily for 1 to 7 days, depending on the severity of the infection.
- Effectiveness: Miconazole is a first-line treatment for vaginal thrush and is effective for most cases.
- Side effects: Mild irritation, burning, or itching at the application site may occur.
Amphotericin B
- Dosage: Amphotericin B is used for severe systemic candidiasis and is administered intravenously in a hospital setting. Dosage depends on the severity of the infection and the patient’s condition.
- Effectiveness: Amphotericin B is effective for treating life-threatening fungal infections, including systemic candidiasis.
- Side effects: Side effects can be significant and include fever, chills, kidney toxicity, and low potassium levels.
Where is Thrush Most Prevalent?
Thrush is a common infection that occurs worldwide, but certain factors make it more prevalent in specific regions, populations, and environments.
Global Prevalence
Thrush is a global health issue, affecting millions of people each year. While it can occur in anyone, it is particularly prevalent in populations with compromised immune systems, such as those living with HIV/AIDS. Areas where access to healthcare is limited, and hygiene practices are suboptimal, tend to see higher rates of thrush and other fungal infections.
- Developed countries: In developed countries, thrush is most commonly seen in vulnerable populations such as infants, elderly individuals, and people undergoing treatments that suppress the immune system (e.g., chemotherapy, corticosteroids).
- Developing countries: In developing countries, particularly in regions with high rates of HIV/AIDS, thrush is more prevalent due to the immunosuppressive nature of the virus. Lack of access to proper healthcare and antifungal treatments can make the infection more severe and widespread.
Populations at Higher Risk
Certain populations are more susceptible to thrush due to various risk factors, including:
- Infants and breastfeeding mothers: Oral thrush is common in infants, particularly those who are breastfed. Candida can spread between the mother’s nipples and the baby’s mouth.
- Immunocompromised individuals: People with weakened immune systems, such as those with HIV/AIDS, cancer patients, and transplant recipients, are more vulnerable to severe or recurrent thrush.
- Diabetics: Individuals with poorly controlled diabetes are at higher risk of developing both oral and vaginal thrush due to elevated blood sugar levels, which promote the growth of Candida.
Environmental and Cultural Factors
Certain environmental and cultural factors can also contribute to the prevalence of thrush:
- Warm, humid climates: Thrush and other fungal infections are more common in warm, humid environments where Candida thrives.
- Communal living: In regions where people live in close quarters, such as refugee camps or communal housing, thrush can spread more easily due to shared hygiene facilities and limited access to healthcare.
Prevention of Thrush
Preventing thrush involves maintaining good hygiene, managing underlying health conditions, and avoiding factors that can disrupt the balance of microorganisms in the body.
Good Oral and Vaginal Hygiene
Proper hygiene is essential in preventing the overgrowth of Candida and the development of thrush.
- Brush teeth regularly: Brushing your teeth at least twice a day and flossing daily can help prevent oral thrush by removing food particles and bacteria that can contribute to yeast overgrowth.
- Clean dentures properly: For people who wear dentures, it is important to clean them thoroughly and remove them at night to reduce the risk of oral thrush.
- Avoid douching: For women, avoiding vaginal douching is important, as it can disrupt the natural balance of bacteria and yeast, leading to vaginal thrush.
Control of Underlying Conditions
Managing underlying health conditions can reduce the risk of thrush, particularly in individuals with diabetes or compromised immune systems.
- Manage blood sugar levels: Diabetics should monitor and control their blood sugar levels to reduce the risk of Candida overgrowth.
- Strengthen the immune system: People with weakened immune systems should work with their healthcare providers to optimize their overall health and take preventive measures to avoid infections.
Limiting Antibiotic and Steroid Use
Antibiotics and corticosteroids can disrupt the natural balance of microorganisms in the body, increasing the risk of thrush.
- Use antibiotics cautiously: Only take antibiotics when prescribed by a healthcare provider, and complete the full course to prevent the overgrowth of fungi.
- Rinse mouth after steroid inhalers: People who use steroid inhalers for asthma should rinse their mouths thoroughly after each use to reduce the risk of oral thrush.
Diet and Lifestyle
Certain dietary and lifestyle changes may help prevent thrush:
- Limit sugar intake: High-sugar diets can promote the growth of Candida, so reducing sugar and refined carbohydrates in your diet can help lower the risk of thrush.
- Wear breathable fabrics: For individuals prone to vaginal thrush, wearing breathable, cotton underwear and loose-fitting clothing can help keep the area dry and prevent yeast overgrowth.
Probiotics
Some studies suggest that probiotics may help prevent thrush by promoting a healthy balance of bacteria and yeast in the body, particularly after antibiotic use. While more research is needed, probiotics may be beneficial for individuals at risk of recurrent thrush.
Regular Medical Checkups
People with compromised immune systems or other risk factors should have regular medical checkups to monitor for signs of thrush and other infections. Early detection and treatment can prevent the infection from becoming more serious.

