Tuberculosis: Symptoms, Treatments, Medications and Prevention
Tuberculosis (TB) is a bacterial infection caused by Mycobacterium tuberculosis, primarily affecting the lungs but can also impact other organs in the body. Although TB was once a major public health issue in many parts of the world, advances in antibiotics have significantly reduced the prevalence of the disease in developed nations. However, it remains a serious global health concern, particularly in low- and middle-income countries.
What is Tuberculosis?
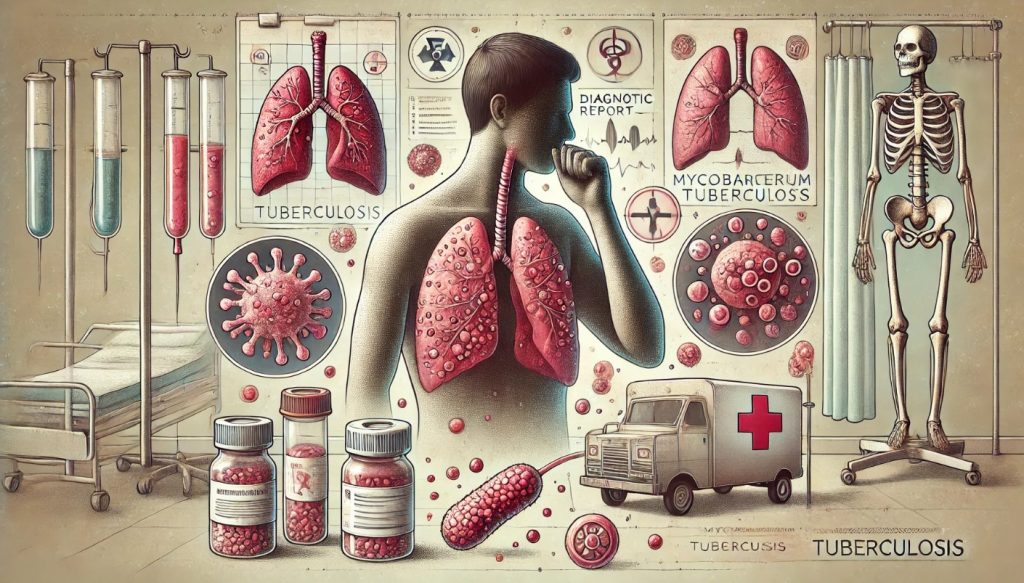
Tuberculosis is a highly contagious airborne disease that primarily affects the lungs but can also spread to other parts of the body, including the kidneys, spine, and brain. TB is caused by the bacterium Mycobacterium tuberculosis, which spreads through microscopic droplets released into the air when an infected person coughs, sneezes, speaks, or sings. While TB can be fatal if left untreated, it is both preventable and curable with proper medical care.
Forms of Tuberculosis
Tuberculosis can present itself in two main forms:
- Latent TB Infection (LTBI): In this form, a person is infected with Mycobacterium tuberculosis, but the bacteria remain inactive in the body. Individuals with latent TB do not exhibit symptoms and are not contagious. However, if left untreated, latent TB can develop into active TB, especially if the person’s immune system weakens.
- Active TB Disease: Active TB occurs when the bacteria multiply and cause symptoms. This form is contagious and can spread to others. It is more common in people with weakened immune systems, such as those with HIV or those taking immunosuppressive medications.
Transmission
TB spreads when an infected person releases TB bacteria into the air, typically by coughing, sneezing, or speaking. People nearby can inhale these bacteria and become infected. TB is more likely to spread in environments where individuals are in close contact over long periods, such as households, workplaces, or healthcare settings. However, TB is not easily spread through casual contact, like shaking hands or sharing food.
Who is at Risk of Tuberculosis?
While anyone can become infected with tuberculosis, certain populations are at a higher risk due to a combination of biological, environmental, and socioeconomic factors. Understanding who is most vulnerable is key to implementing effective prevention and treatment strategies.
High-Risk Groups for TB Infection
- Individuals with Compromised Immune Systems: People with weakened immune systems are more susceptible to TB because their bodies are less capable of fighting off infections. This includes individuals with:
- HIV/AIDS: People with HIV are 18 times more likely to develop active TB than those without HIV.
- Cancer patients undergoing chemotherapy
- Individuals receiving immunosuppressive treatments for conditions like autoimmune diseases or organ transplants
- People Living in or Traveling to High-Risk Areas: TB is more common in certain regions, especially in developing countries with high poverty levels and limited healthcare access. People living in or traveling to areas with high rates of TB, such as parts of Africa, Asia, Eastern Europe, and Latin America, are at an increased risk.
- Healthcare Workers: Due to frequent contact with infected individuals, healthcare workers, particularly those working in high TB-burden areas, are more likely to be exposed to TB bacteria.
- People Living in Crowded or Poorly Ventilated Environments: TB is more easily transmitted in places where people live in close quarters. This includes:
- Prisons
- Refugee camps
- Shelters for the homeless
- Nursing homes
- Children and Elderly Adults: Young children and the elderly are more vulnerable to TB due to their underdeveloped or weakened immune systems. Children under the age of 5 are particularly at risk for developing severe forms of TB, such as TB meningitis.
- People Who Smoke or Abuse Drugs and Alcohol: Smoking, drug abuse, and excessive alcohol consumption weaken the immune system and damage the lungs, making it easier for TB bacteria to take hold.
Symptoms of Tuberculosis
The symptoms of tuberculosis depend on whether the person has latent TB or active TB disease. In the case of active TB, the symptoms may vary based on which organs are affected, but most commonly, the lungs are involved.
Symptoms of Pulmonary TB (Affecting the Lungs)
- Persistent Cough: A cough lasting more than three weeks is one of the most common symptoms of pulmonary TB. Initially dry, the cough may later produce mucus or blood-streaked sputum.
- Chest Pain: Discomfort or pain in the chest that worsens with breathing or coughing can occur due to the infection’s impact on the lungs.
- Coughing Up Blood (Hemoptysis): In more advanced cases of TB, the infection can cause damage to the lungs, leading to blood in the sputum.
- Fatigue and Weakness: TB often causes general fatigue, weakness, and a lack of energy due to the body’s immune response to the infection.
- Weight Loss and Loss of Appetite: Unexplained weight loss and a reduced appetite are common in individuals with active TB.
- Fever and Chills: A low-grade fever, often accompanied by chills or night sweats, is typical of TB, especially in the evenings.
- Night Sweats: Many individuals with TB experience drenching night sweats, a result of the body’s immune system fighting the infection.
Extrapulmonary TB Symptoms
In cases where TB affects organs other than the lungs (extrapulmonary TB), symptoms vary depending on the organ involved:
- TB Meningitis: Symptoms may include headaches, neck stiffness, sensitivity to light, and altered mental status.
- TB in the Kidneys: Kidney TB can cause flank pain, blood in the urine, and a decreased frequency of urination.
- TB of the Bones and Joints: This can cause severe pain and swelling in the affected bones or joints, often affecting the spine (Pott’s disease).
Latent TB Symptoms
Latent TB is asymptomatic, meaning that individuals with this form of the infection show no symptoms and do not feel ill. However, the infection can become active, especially in people with weakened immune systems.
Diagnosis of Tuberculosis
Diagnosing tuberculosis can be challenging because many of its symptoms overlap with other respiratory conditions, such as pneumonia or chronic bronchitis. Various diagnostic tools and tests are used to confirm TB infection and differentiate between latent and active forms.
Initial Screening Tests
- Tuberculin Skin Test (TST): Also known as the Mantoux test, this screening tool involves injecting a small amount of purified protein derivative (PPD) under the skin. After 48-72 hours, the injection site is examined for a reaction, such as redness or swelling. A positive result indicates TB exposure, but further tests are needed to confirm active infection.
- Interferon-Gamma Release Assays (IGRAs): Blood tests like the QuantiFERON-TB Gold and T-SPOT.TB are used to detect TB infection by measuring the immune system’s response to TB antigens. These tests are more specific than the TST and are especially useful for people who have received the BCG vaccine (a TB vaccine given in many countries).
Diagnostic Tests for Active TB
If TB infection is suspected, additional tests are required to confirm the diagnosis and determine the extent of the disease.
- Sputum Smear Microscopy: Sputum samples (mucus coughed up from the lungs) are examined under a microscope to detect the presence of Mycobacterium tuberculosis. A positive sputum smear confirms active pulmonary TB.
- Chest X-Ray: A chest X-ray is often used to identify abnormalities in the lungs that suggest TB, such as cavities, scarring, or nodules. While an X-ray can indicate TB, it cannot confirm the diagnosis alone.
- Sputum Culture: This test involves growing TB bacteria from a sputum sample in a laboratory. While it is the most accurate test for diagnosing TB, it can take several weeks for results because TB bacteria grow slowly.
- Nucleic Acid Amplification Tests (NAATs): These tests detect TB DNA in sputum samples. They are faster than cultures and can also test for drug resistance, such as resistance to rifampicin, a key TB drug.
- Biopsy or Tissue Sample Analysis: In cases of extrapulmonary TB, a biopsy may be performed on affected tissues, such as lymph nodes, to confirm the presence of TB bacteria.
- Lumbar Puncture (Spinal Tap): In cases of suspected TB meningitis, a lumbar puncture is used to collect cerebrospinal fluid for analysis.
Treatment of Tuberculosis
Tuberculosis is treatable and curable, but it requires a prolonged course of antibiotics to ensure that the bacteria are completely eradicated. Inadequate or incomplete treatment can lead to drug-resistant strains of TB, which are much more difficult to treat.
Standard TB Treatment (Drug-Sensitive TB)
The most common treatment for drug-sensitive TB is a combination of four first-line antibiotics, taken over a period of six to nine months. The initial two-month intensive phase is followed by a continuation phase lasting four to seven months, depending on the patient’s response to treatment.
- Intensive Phase: During the first two months, patients typically take four drugs:
- Isoniazid (INH): A powerful bactericidal drug that kills rapidly dividing TB bacteria.
- Rifampicin (RIF): This drug inhibits bacterial RNA synthesis and is crucial for preventing relapses.
- Pyrazinamide (PZA): Particularly effective in killing dormant TB bacteria in acidic environments, such as within granulomas.
- Ethambutol (EMB): This drug helps prevent drug resistance and is used until the bacteria are confirmed to be susceptible to the other drugs.
- Continuation Phase: After the initial two months, patients typically continue with two drugs—isoniazid and rifampicin—for an additional four to seven months. This phase ensures the complete eradication of the bacteria.
Treatment for Drug-Resistant TB
Multidrug-resistant TB (MDR-TB) occurs when the bacteria become resistant to at least isoniazid and rifampicin, the two most potent first-line drugs. Treating MDR-TB requires the use of second-line drugs, which are often less effective, more expensive, and come with more severe side effects. Treatment for MDR-TB can last 18 to 24 months or longer.
- Second-Line Drugs: Treatment regimens for MDR-TB often include drugs like:
- Fluoroquinolones: Such as levofloxacin or moxifloxacin, which are potent antibiotics used in MDR-TB treatment.
- Injectable Medications: Such as amikacin, kanamycin, or capreomycin.
- Newer Drugs: In recent years, newer drugs like bedaquiline and delamanid have been developed for treating drug-resistant TB and are showing promising results.
- Extensively Drug-Resistant TB (XDR-TB): This is a rare form of MDR-TB that is resistant to nearly all antibiotics used to treat TB, including the most potent second-line drugs. Treating XDR-TB is extremely challenging and often requires the use of experimental drugs or surgical interventions to remove infected tissue.
Most Common Medications for Tuberculosis
The cornerstone of TB treatment lies in the use of antibiotics, and the choice of drugs depends on whether the TB strain is drug-sensitive or drug-resistant.
First-Line Medications (For Drug-Sensitive TB)
- Isoniazid (INH): Isoniazid is one of the most important drugs in TB treatment. It works by killing actively dividing bacteria and is typically given daily or three times a week.
- Rifampicin (RIF): Rifampicin is a critical drug in TB treatment because it kills bacteria by inhibiting RNA synthesis, preventing the bacteria from multiplying. It is also a key drug in preventing the relapse of TB after initial treatment.
- Pyrazinamide (PZA): This drug is particularly effective during the early stages of TB treatment, especially against dormant bacteria hiding in the acidic environment of the body’s granulomas.
- Ethambutol (EMB): Ethambutol prevents the bacteria from developing resistance to other TB drugs by inhibiting cell wall synthesis. It is typically used during the initial intensive phase of treatment.
Second-Line Medications (For Drug-Resistant TB)
When first-line treatments are ineffective due to drug resistance, second-line antibiotics are used:
- Fluoroquinolones: Levofloxacin and moxifloxacin are powerful antibiotics often used in the treatment of MDR-TB.
- Aminoglycosides: Amikacin and kanamycin are injectable antibiotics that are used when the TB strain is resistant to first-line drugs.
- Bedaquiline and Delamanid: These newer medications are used to treat MDR-TB and XDR-TB. They are highly effective but are generally reserved for cases where other drugs have failed.
Where is Tuberculosis Most Prevalent?
Tuberculosis is a global disease but is more prevalent in certain regions of the world, particularly in low- and middle-income countries where access to healthcare is limited, and living conditions contribute to the spread of the disease.
Geographic Regions with High TB Burden
- Sub-Saharan Africa: Countries in sub-Saharan Africa have some of the highest rates of TB in the world. This is due to a combination of poverty, overcrowded living conditions, and the high prevalence of HIV, which significantly increases the risk of developing active TB.
- South and Southeast Asia: Countries like India, Indonesia, Bangladesh, and the Philippines have high TB rates, contributing to a significant portion of the global TB burden. In these regions, poor healthcare infrastructure and limited access to diagnostic and treatment facilities exacerbate the spread of TB.
- Eastern Europe: Several countries in Eastern Europe, particularly the former Soviet states, have high rates of MDR-TB and XDR-TB. Poor management of TB cases, combined with socioeconomic instability, has led to a surge in drug-resistant forms of the disease in these areas.
- Latin America: While TB rates are lower in Latin America compared to Africa and Asia, countries such as Brazil and Peru still face significant challenges in controlling the disease, particularly in rural and underserved areas.
Social and Economic Factors Contributing to TB Prevalence
- Poverty: Poverty is a key factor in the spread of TB. People living in poverty often have limited access to healthcare, poor nutrition, and live in overcrowded conditions, all of which increase the risk of TB transmission.
- HIV Co-Infection: In many regions, particularly sub-Saharan Africa, the high prevalence of HIV/AIDS contributes to higher TB rates. People with HIV are much more likely to develop active TB due to their compromised immune systems.
- Lack of Healthcare Access: In many high TB-burden regions, healthcare systems are underfunded and understaffed. This leads to delayed diagnosis, inadequate treatment, and higher rates of drug-resistant TB.
Prevention of Tuberculosis
Preventing tuberculosis is a critical public health challenge, particularly in regions with high TB rates. Strategies for TB prevention involve a combination of vaccination, public health initiatives, infection control measures, and targeted treatment of latent TB.
Vaccination
- BCG Vaccine: The Bacillus Calmette-Guérin (BCG) vaccine is the only available vaccine for TB. It is most effective at preventing severe forms of TB in children, such as TB meningitis and miliary TB. However, it is less effective at preventing pulmonary TB in adults, and it is not widely used in countries with low TB incidence. The BCG vaccine is typically administered to newborns in high-burden countries.
Public Health Measures
- Early Detection and Treatment: One of the most effective ways to prevent TB is to detect and treat active TB cases as early as possible. This not only helps cure the patient but also reduces the risk of transmission to others. Screening programs, particularly in high-risk populations, are critical to identifying TB cases early.
- Treatment of Latent TB Infection (LTBI): People with latent TB are at risk of developing active TB, especially if they have weakened immune systems. Treating latent TB with preventive antibiotics (usually isoniazid or rifapentine) can significantly reduce the risk of progression to active disease.
- Infection Control in Healthcare Settings: In hospitals and clinics, strict infection control measures are essential to prevent the spread of TB. This includes isolating patients with active TB, ensuring proper ventilation, and providing healthcare workers with protective equipment, such as N95 masks.
- Improving Living Conditions: Addressing the social determinants of TB, such as poverty, overcrowded housing, and poor nutrition, is critical for preventing the spread of the disease. Governments and organizations need to invest in improving housing conditions and access to healthcare services in high-burden areas.
Reducing TB Transmission in High-Risk Groups
- HIV Testing and Treatment: Because HIV significantly increases the risk of developing active TB, routine testing for HIV in TB patients is essential. Additionally, providing antiretroviral therapy (ART) to people living with HIV can strengthen the immune system and reduce the risk of TB.
- Avoiding Exposure in High-Risk Environments: People at higher risk of TB, such as healthcare workers or individuals living in crowded settings, should take precautions to avoid exposure to TB bacteria. This may include using personal protective equipment (PPE) and following strict infection control protocols.
Community-Based Prevention Strategies
In regions with high TB incidence, community-based interventions can play a crucial role in reducing the spread of the disease. These strategies include:
- Education and Awareness Campaigns: Raising awareness about TB, its symptoms, and how it spreads can encourage early diagnosis and treatment. Educational campaigns are particularly effective in communities with low health literacy.
- Directly Observed Therapy (DOT): This strategy involves healthcare workers or trained community members observing TB patients as they take their medication. This ensures that patients complete their full course of treatment, reducing the risk of drug resistance and preventing relapse.
